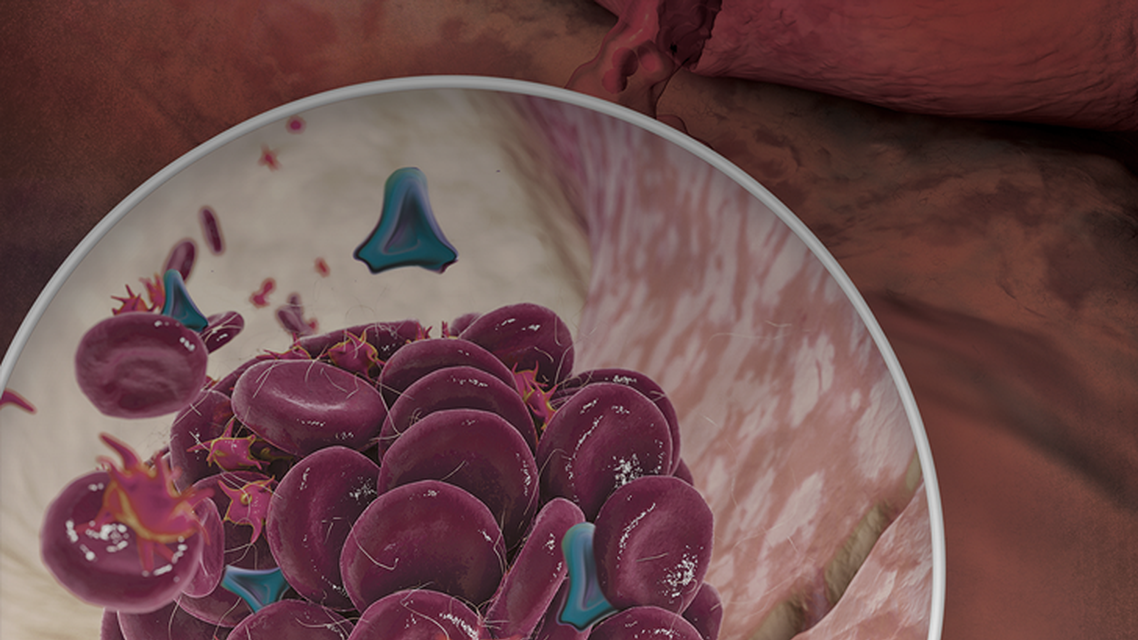
Hemophilia A is an inherited or spontaneously occurring secondary hemostasis disorder caused by clotting factor VIII deficiency, which affects the formation and stabilization of clots. If left untreated, hemophilia A can cause recurrent and disabling bleeding, leading to severe arthropathy or life- threatening hemorrhage. Prophylaxis is well-documented for its effectiveness in preventing arthropathy and life-threatening bleeds, and improving total bleeding rates. However, limitations of modern factor replacement treatment result in suboptimal outcomes, poor adherence to prophylactic regimens, and reduced QoL. Novel and emerging prophylactic therapies can mitigate some of the hindrances of traditional replacement therapy and enhance the overall effect of treatment in hemophilia A.
In this educational activity, expert faculty will review recent evidence from key clinical trials of prophylactic therapies that are expanding the armamentarium of therapeutic choices, including a novel high-sustained factor VIII replacement therapy, a bispecific antibody non-factor replacement therapy, and other emerging therapies. Evaluating patients’ goals and preferences will also be discussed, so clinicians can co-create treatment plans using a shared decision approach to improve adherence and reduce bleeding episodes in patients with hemophilia A.

 In support of improving patient care, AXIS Medical Education is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
In support of improving patient care, AXIS Medical Education is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.  This activity was planned by and for the healthcare team, and learners will receive 0.5 Interprofessional Continuing Education (IPCE) credit for learning and change.
This activity was planned by and for the healthcare team, and learners will receive 0.5 Interprofessional Continuing Education (IPCE) credit for learning and change. AXIS Medical Education has been authorized by the American Academy of PAs (AAPA) to award AAPA Category 1 CME credit for activities planned in accordance with AAPA CME Criteria. This activity is designated for 0.5 AAPA Category 1 CME credits. Approval is valid until August 16, 2024 PAs should only claim credit commensurate with the extent of their participation.
AXIS Medical Education has been authorized by the American Academy of PAs (AAPA) to award AAPA Category 1 CME credit for activities planned in accordance with AAPA CME Criteria. This activity is designated for 0.5 AAPA Category 1 CME credits. Approval is valid until August 16, 2024 PAs should only claim credit commensurate with the extent of their participation.










Facebook Comments