Announcer:
Welcome to CME on ReachMD. This episode is part of our MinuteCE curriculum.
Prior to beginning the activity, please be sure to review the faculty and commercial support disclosure statements as well as the learning objectives.
Dr. Moses:
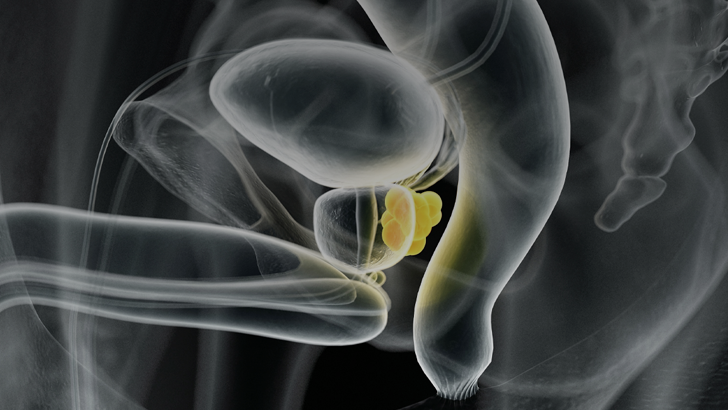
Hello, I'm Kelvin Moses, Associate Professor of Urology at Vanderbilt University Medical Center. And I'm thankful for you joining me for our topic, What Can I Do to Improve Care of Prostate Cancer Patients at Risk for Inequities?
Just to understand the landscape of prostate cancer among African American men, there are disparities on all points of the prostate cancer continuum. And so that goes all the way from screening and treatment to outcomes and death from prostate cancer. There are several factors that contribute to this, including lack of diversity in the physician workforce, lack of diversity and funding agency leadership and study sections, and also a lack of participation of black men in clinical trials, which leads to deprioritization of what is otherwise a glaring public health crisis. There are several decades of descriptive analyses about disparities in prostate cancer. But right now, we need more information on how do we reduce these disparities with action?
So black men who have more than double the risk of death from prostate cancer compared to white men, and are more likely to be diagnosed with higher grade and stage disease, but also less likely to receive treatment for prostate cancer and be diagnosed at an earlier age. When we talk about less screening, black men are less likely to receive screening in the form of PSA or rectal exam, and either received no treatment at all or more likely to receive radiation in comparison to surgery.
In a study that we performed several years ago, we showed that African American men actually have lower odds of receiving any type of therapy, even for higher risk disease compared to white men. And for Hispanic men, even for intermediate or high-risk disease, are still less likely to receive treatment. And this is a problem in that a lot of the disparity has to do with lack of appropriate treatment in men.
When talking about clinical trials, we see some of the recent trials in metastatic hormone-sensitive cancer like TITAN, ENZAMET, ARCHES, and ARASENS. And as you can see here, the total number of African American men enrolled represents less than 3% of all of the patients involved. And this is where trials that actually report on the presence of African American men, many trials did not even address this. And so again, this reiterates the point that we need to improve and actually oversample for African American men in prostate cancer clinical trials, due to the higher mortality.
One of the other factors that leads to disparities and outcome are what are called social determinants of health. And these are the non-medical factors which describe the environment and circumstances in which we all live and work. This impacts everyone, and not necessarily positive or negative. But you can see on the graphic here, some of the factors that go into determination of health and social needs. Some of these needs have to do with socioeconomic. So if patients have a job, if they have an income, if they have insurance, but also some of their support system, their neighborhood, their family support. People's individual preferences and priorities should be noted because these do play a role in identifying not only some of the interventions needed for treatment, but social interventions that may be needed as well.
So here's our call to arms, we’re capable, as physicians, to recognize shortcomings in our practices. And we can look at the opioid crisis and how we've been involved with that. Advocacy for black men doesn't just occur in the clinical setting. And I point out the IMPACT program in California, where men without insurance could get treatment for prostate cancer from state funds. So now is the time for action in our highest risk populations.
So what can we do? We need to understand the historical context of disparities and why they happen. We need to encourage community partnerships between our healthcare centers and local community at the grassroots level. We need to actively recruit black men into clinical trials and discuss strategies for development with our industry and cooperative groups as well as with the NCI. We need to promote expansion for care in uninsured and underinsured men in academic and community practices. And that involves aligning our political activity for the best outcomes for vulnerable patients. And lastly, we need to advocate for diversity in the medical field and elevate cultural competency among all physicians.
I thank you for your attention to this important topic. And we'll see you later.
Announcer:
You have been listening to CME on ReachMD. This activity is jointly provided by Global Learning Collaborative (GLC) and TotalCME, LLC. and is part of our MinuteCE curriculum.
To receive your free CME credit, or to download this activity, go to ReachMD.com/CME. Thank you for listening.

 In support of improving patient care, this activity has been planned and implemented by Global Learning Collaborative (GLC) and Total CME, LLC. GLC is jointly accredited by the American Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC) to provide continuing education for the healthcare team.
In support of improving patient care, this activity has been planned and implemented by Global Learning Collaborative (GLC) and Total CME, LLC. GLC is jointly accredited by the American Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC) to provide continuing education for the healthcare team.


Facebook Comments